Oraltide Pro™ − the latest peptide technology for dental care
May 17th, 2019By Leslie J. Farer
Oral health is essential to overall health, yet many overlook this important fact when devising an anti-aging protocol. Poor dental health can lead to a range of problems throughout the body including cardiovascular disease, cancer, arthritis, and other degenerative diseases that undermine the prospect of a long and healthy life. Although practicing good dental hygiene is of utmost importance, often more help is needed for teeth and gums to maintain their optimal integrity (as well as appearance).
Recent advances in dentistry have led to the development of the Oraltide-Pro™ line of products − concentrated mouthwash, and an intensive repair gel − to target two major issues in dental health: tooth decay due to erosion of protective enamel and gum recession due to periodontal disease. Oraltide-Pro™ products employ innovative peptide technology to treat these issues, allowing you to improve and maintain the health of your teeth and gums with products you can use at home.
In this article, we’ll cover enamel erosion and gum recession, their development and progression, and treatments for each, including conventional as well as cutting-edge techniques upon which Oraltide™ products are based.
Enamel 101
The protective mineralized enamel covering teeth is the hardest substance in the body, even harder than bone. But in spite of its strength, it can’t always stand up to years of wear and tear and degradation due to consumption of sugar-laden food and drinks. When enamel wears away, teeth become more susceptible to sensitivity, decay, and cavities. Unlike bone, the body doesn’t have mechanisms to regenerate enamel; once it’s gone it can’t be replaced. However, as we’ll see below, certain substances repair, or “fill in,” small surface lesions that form as enamel erodes, thereby strengthening the structure of existing enamel and protecting teeth from further damage.
Enamel is primarily composed of the mineral hydroxyapatite (crystalline calcium phosphate, Ca10 (PO4)6 (OH)2). The main culprit in enamel loss is acid, specifically, the formation of organic acids from the metabolism of carbohydrates (such as refined carbohydrates, including sugar in sweets, soft drinks, and fruit juice) by bacteria residing in a substance called plaque, which is a sticky biofilm covering teeth. When exposed to low pH, hydroxyapatite crystals forming the structural backbone of enamel break down − literally dissolve −into calcium and phosphate ions in a process known as demineralization, resulting in the formation of lesions or crystal voids on the tooth’s surface. This degradation is temporarily reversible by a naturally occurring remineralization process in which calcium and phosphate ions are diffused from saliva back onto the tooth’s surface and deposited into crystal voids to restore the lost structure.
Enamel remineralization and demineralization is an on-going dynamic process. Problems occur when the dynamic is shifted toward demineralization, which leads to permanent enamel loss and its consequences: tooth decay due to bacterial invasion deeper into the tooth, cavities, sensitivity resulting from the exposure of dentin (the layer below enamel), and further structural decline including cracks, chips, and fractures (not to mention unsightly tooth discoloration and chipped, cracked teeth). The good news is, there are steps you can take to favor remineralization, including dietary modifications limiting sugar and refined carbohydrates, regular dental checkups and biannual cleanings, and daily brushing and flossing, in addition to specialized treatments and products.
Enamel remineralization treatments
Fluoride treatments and fluoride toothpastes and mouthwashes have been widely touted as effective in promoting the diffusion of calcium and phosphate ions back onto the tooth surface to fortify the enamel crystalline structure, resulting in the formation of fluoridated hydroxyapatite and fluorapatite, instead of natural hydroxyapatite. Although the resulting re-mineralized tooth surfaces are stronger and more acid resistant than the original teeth, critics believe fluoride to be potentially toxic. According to the International Academy of Oral Medicine and Toxicology, fluoride exposure at levels currently thought to be safe can cause damage to the cardiovascular, nervous, endocrine, immune, and skeletal systems, and has been linked to diseases such as Alzheimer’s, cancer, diabetes, and heart disease. (1)
Recent advancements in dentistry for enamel strengthening (and alternatives to fluoride) encourage natural hydroxyapatite mineralization, include the compound casein phosphopeptide-amorphous calcium phosphate (CPP-ACP), a key ingredient in Oraltide-Pro™.
Casein phosphopeptides (CPP’s) are a group of peptides derived from milk protein casein with the ability to markedly increase the solubility and bioavailability of calcium phosphate to produce a form known as ‘amorphous calcium phosphate’ (ACP). (2) ACP is a precursor in the formation of hydroxyapatite, making it a valuable remineralizing agent. In the past, the use of un-complexed calcium phosphate for remineralization was ineffective due to its low water solubility resulting in low concentrations delivered to the tooth surface. But now, this new technology using CPP to facilitate high, even supersaturated concentrations of calcium and phosphate ions, has shown much success.
CPP-ACP binds readily to the surface of the tooth where it deposits a high concentration of ACP, (2-4) repairing lesions in enamel and protecting against acid erosion. Several studies show that ACP fights tooth decay in animals and humans (5,6) by increasing the resistance of enamel.
Mineralization of crystal voids to fortify existing enamel and prevent further damage is far preferable to more aggressive techniques that become necessary once enamel is past the point of lesion repair, such as bonding (in which resin is applied to the tooth with eroded enamel, then trimmed and polished) or crowns or veneers (which involve capping the damaged tooth).
When it comes to strengthening enamel and protecting against tooth decay and sensitivity, fluoride-free Oraltide-Pro™ is a great choice − they incorporate the proven mineralizing treatment CPP-ACP into dental care products you can use at home − safely.
Gingival recession – not just an aesthetic concern
Besides restoring and maintaining the structural integrity of enamel to prevent tooth decay, Oraltide-Pro™ also targets another major issue in dental health − gingival (gum) recession, a condition in which the immediate gum tissue surrounding teeth recedes or pulls back, exposing the lower part of the tooth and root. Gum recession is common, especially with age − it’s estimated that over 60 percent of the human population has it. (7) Besides its unattractive appearance, gingival recession may be an indicator of deeper problems.
Gingivitis, the first step in the development of periodontal disease, is an inflammation of gum tissue caused by bacterial build-up in plaque. If caught in time, gingivitis can be treated and reversed with proper plaque control, (i.e., dental cleanings at least twice a year, daily brushing and flossing, and antibacterial mouthwashes); otherwise it may progress to the more serious periodontitis.
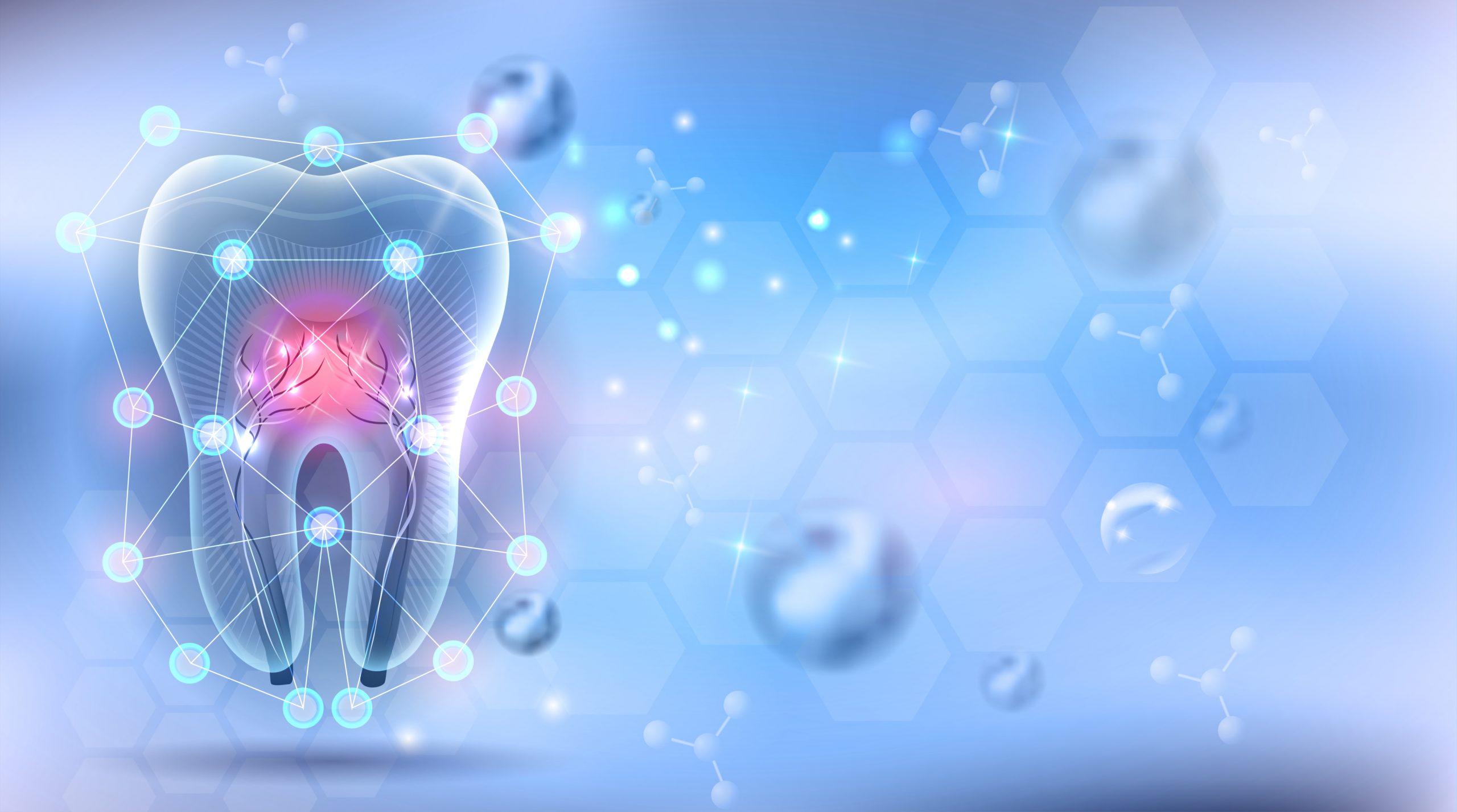
In periodontitis, the inner layer of gum and bone pull away from teeth forming deep pockets that harbor tissue-destroying bacteria as plaque spreads below the gum line (see figure 1). As the disease progresses, the alveolar bone, (a thin layer of bone that forms the sockets around the roots of the teeth) and connective tissue, including the periodontal ligamentsthat anchor teeth in place degenerate, resulting in loose teeth, and potentially permanent loss of teeth. Periodontal disease should be treated as soon as detected (preferably prevented in the first place), since besides causing gum, bone, and tooth loss, it may lead to systemic inflammation and a range of illnesses throughout the body, including cancer, heart disease, diabetes, arthritis, and others.
Besides periodontal disease, other factors leading to the development of receding gums include genetic predisposition, overly aggressive tooth brushing, (which causes damage to both enamel and gums), poor dental hygiene (i.e., inadequate brushing and flossing, and infrequent dental checkups and cleanings), teeth grinding and smoking.
Treatments for gingival recession
There are a variety of conventional and recently developed regenerative methods to alleviate gum recession.
First let’s look at the conventional treatments. In mild cases, dentists often perform a ‘deep cleaning’ procedure called ‘tooth scaling and root planing’ to remove harmful bacteria-containing plaque on teeth and below the gum line and smooth irregular root surfaces. For more advanced recession, surgery is often necessary to cover the exposed root. ‘Open flap scaling and root planing’ involves folding back gum tissue, removing bacteria and plaque from pockets, and then tightening and securing gum tissue over teeth to remove or shrink pockets. Soft tissue grafts are another commonly used procedure in which tissue taken from underneath the palate (roof) of the mouth, or from the palate itself is grafted to gum tissue surrounding a tooth’s exposed root. Although these conventional methods may slow the progression of periodontal disease by removing bacteria, reducing pockets, or covering the exposed areas with soft tissue grafts, they do not improve the overall health of the supportive tissue structures.
Now we’ll examine state-of-the-art methods that treat and even reverse gingival recession by actively promoting the regeneration of damaged or lost tissues.
In recent years, great strides have been made in a fascinating area known as regenerative medicine that uses techniques such as implanting a membrane or scaffold seeded with a patient’s own cells or applying tissue-stimulating proteins or other biologically active molecules to the affected area to jumpstart the body’s innate healing mechanisms for the purpose ofrebuilding ‘from scratch’ functional tissue to replace damaged or lost bone or tissue. Regenerative medicine has multiple applications in rebuilding organs and tissues system-wide, such as skin, cartilage, kidneys, liver, etc., as well as periodontal supportive structures including bone and gingival tissue.
Several studies show that grafts engineered from various types of scaffolds and cell types are a viable, if not superior alternative to the soft tissue grafts discussed above. For example, in one such study, membranes seeded with patients’ own gingival-derived cells initiated the regeneration of receding gums. Tissue-engineered grafts were created by culturing a small portion of a patient’s gum tissue. Fibroblasts (cells involved in wound healing and tissue repair − we’ll see more on fibroblasts below) derived from the cell culture were then infused onto a membrane, which was trimmed to fit the affected root area and sutured to adjacent gum tissue underneath a ‘flap’ that completely covered the graft. Within weeks, the fibroblast-seeded membrane triggered the growth of new, disease-free gingival tissue in the area previously marked by recession. (8)
In addition to tissue-engineered grafts, periodontal tissues can be reconstructed using growth factors, specialized signaling molecules that mediate wound healing and tissue repair. There are a variety of growth factor types such as vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), and transforming growth factor (TGF), that interact with cells and other growth factors to ‘orchestrate’ growth and repair processes such as cell proliferation, extracellular matrix production,and collagen synthesis. The extracellular matrix is a network of carbohydrates and fibrous proteins including collagen that surrounds cells to form a mesh or network providing structural support to tissues. During wound healing, fibroblasts (the cell type seeded onto the tissue-engineered grafts described above) migrate to the wound site, proliferate, and are stimulated by certain growth factors to generate the collagen-containing extracellular matrix necessary for new tissues.
These key processes − extracellular matrix and collagen production by fibroblasts in response to cell signaling by growth factors − are among the most important ones that researchers experimentally manipulate in order to repair damaged or create new tissues. Several studies have examined the use of growth factors to initiate tissue generation, including periodontal tissues. In vitro studies show that TGF-β (a subtype of TGF) stimulates collagen production and cell proliferation (necessary for tissue generation) in human and animal gingival fibroblasts and periodontal ligament cells. (9) In humans, a placebo-controlled clinical trial on 253 patients with periodontitis demonstrated that topical application of another growth factor, FGF-2 (an FGF subtype) to alveolar bone regenerated periodontal tissue that had been destroyed by periodontitis. (10)
Oraltide-Pro™ products are based on regenerative medicine techniques
These studies are among a multitude that demonstrate the power of regenerative medicine to rebuild tissues, including periodontal supportive structures. Now this potential can be harnessed in products that you can use at home as part of your routine daily dental care regimen.
Instead of a fibroblast-seeded membrane implant, or the direct application of growth factors to periodontal tissue to initiate regeneration, Oraltide-Pro™ works by an alternate, though similar mechanism. The products contain two peptides, palmitoyl pentapeptide-4 and palmitoyl hexapeptide-12, which stimulate gene expression of TGF-β and the resulting biosynthesis of the extracellular matrix and collagen by fibroblasts. (11) Rather than applying growth factors directly to degenerating periodontal tissues, as we saw in the clinical study above, Oraltide-Pro™ works by orally delivering peptide ‘stimulators’ of growth factors which spur the body’s own production of TGF-β, activating fibroblasts to proliferate and do their job of tissue reconstruction (in this case, gingival tissue) − a novel, as well as cost-effective and convenient approach to treating receding gums.
About Oraltide-Pro™ products
The Oraltide-Pro™ product line consists of a concentrated mouthwash and an intensive repair gel. Each product contains the three peptides we’ve discussed: CPP-ACP (for enamel remineralization), palmitoyl pentapeptide-4 and palmitoyl hexapeptide-12 (for gingival regeneration) to simultaneously repair damaged enamel, relieve tooth sensitivity, prevent tooth decay, and rebuild receding gums.
The intensive repair gel also contains xylitol, a natural anti-bacterial and anti-inflammatory sweetener, as well as bicarbonate of soda and coconut oil.
The peptide active ingredients are produced using a patented hydrolysis technology and purified using membrane ultrafiltration. Oraltide-Pro™ products are manufactured from whole food grade raw materials without any harmful ingredients such as fluoride, alcohol, titanium dioxide or chemical bactericides (chlorhexidine, gluconic acid, etc.)
How to use Oraltide-Pro™
Oraltide-Pro™ repair gel
Using it is like a tooth whitening kit, in that the gel is squeezed into a supplied gum shield and then applied onto the teeth. The shield should remain in place for 10-15 minutes. Afterward, the teeth can be brushed and rinsed as usual. This procedure only has to be undertaken once a week.
Oraltide-Pro™ concentrated mouthwash
It can be used once daily, diluted with just one ml of the mouthwash combined with 10 ml water and held in the mouth and circulated for 5 to 10 minutes.
Incorporating both products into your dental care regimen will have a synergistic effect. Also, practicing other critical aspects of good dental hygiene: use a soft-bristled toothbrush, floss daily, make regular appointments for dental exams and cleanings, don’t smoke, and consume a healthy diet (limiting or eliminating refined carbohydrates and sugars).
The Oraltide-Pro™ range is at the leading edge of dental care products employing the latest peptide technologies to restore and promote the integrity of the teeth and gums, which will positively impact not only your dental health, but also your overall health.
More Information:
OraltidePRO Intensive Repair Gel: http://bit.ly/OraltideRepairGel
Oraltide Mouthwash: http://bit.ly/OraltideMouthwashInfo
References
- www.iaomt.org
- Gurunathan D, Somasundaram S, Kumar S. Casein phosphopeptide-amorphous calcium phosphate: a remineralizing agent of enamel. Aust Dent J. 2012 Dec;57(4):404-8.
- Reynolds EC, Cain CJ, Webber FL, et al. Anticariogenicity of calcium phosphate complexes of tryptic casein phosphopeptides in the rat. J Dent Res. 1995;74:1272–1279.
- Reynolds EC, Black CL, Cai F. Advances in enamel remineralization: anticariogenic casein phosphopeptide – amorphous calcium phosphate. J Clin Dent. 1999;10:86–88.
- Cross KJ, Huq NL, Reynolds EC. Casein phosphopeptides in oral health–chemistry and clinical applications. Curr Pharm Des. 2007;13:793–800.
- Reynolds EC. Anticariogenic complexes of amorphous calcium phosphate stabilized by casein phosphopeptides: a review. Spec Care Dentist. 1998;8:8–16.
- Dominiak M, Gedrange T. New Perspectives in the Diagnostic of Gingival Recession. Adv Clin Exp Med. 2014 Nov-Dec;23(6):857-63.
- Jhaveri HM, Chavan MS, Tomar GB, Deshmukh VL, Wani MR, Miller PD Jr. Acellular Dermal Matrix Seeded With Autologous Gingival Fibroblasts for the Treatment of Gingival Recession: A Proof-of-Concept Study. J Periodontol. 2010 Apr;81(4):616-25.
- Takeuchi H, Kubota S, Murakashi E, et al. Effect of transforming growth factor-beta1 on expression of the connective tissue growth factor (CCN2/CTGF) gene in normal human gingival fibroblasts and periodontal ligament cells. J Periodontal Res. 2009 Apr;44(2):161-9.
- Kitamura M, Akamatsu M, Machigashira M, et al. FGF-2 Stimulates Periodontal Regeneration: Results of a Multi-center Randomized Clinical Trial. J Dent Res. 2011 Jan;90(1):35-40.
- Yusen Biotrechnology Co., Ltd. internal document
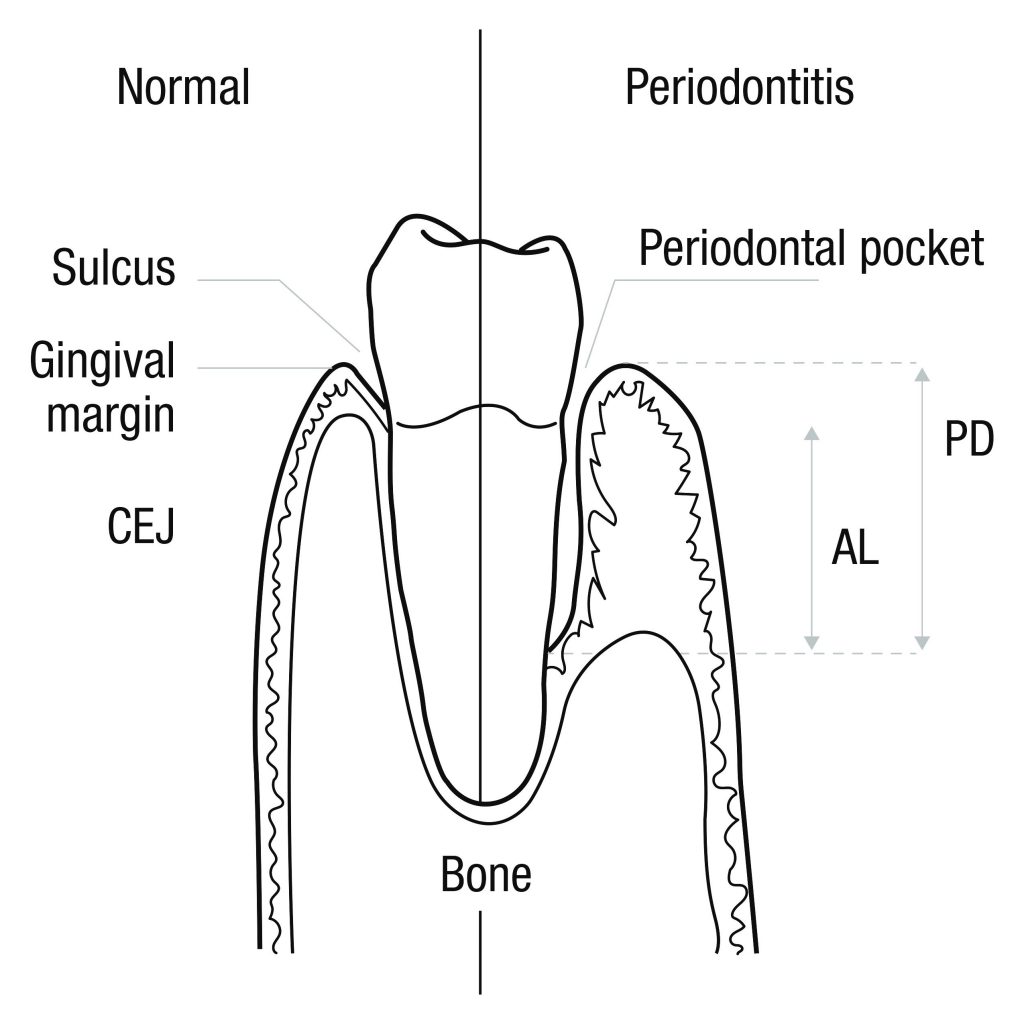
Figure 1: Loss of gum and bone tissue in periodontitis: Ref: openi.nlm.nih.gov