Vitality in Aging
June 4th, 2020By Brian Delaney
For years, my friend and colleague Bill Faloon wanted to create a Manhattan Project–like undertaking to solve aging. Until fairly recently, however, there simply wasn’t enough promising science to give such a project more than the wobbliest of legs to stand on. This changed in the 2010s. Suddenly there were concrete, if tentative, scientific findings in mice and even humans showing that aging could be slowed and, in some ways, even partly reversed.
As the results of studies involving blood-based therapies, senolytics like dasatinib and mTOR inhibitors like rapamycin – to name a couple, it began to look as though aging could be understood and controlled almost completely within a handful of decades, provided enough resources were put to the task. The time was thus nigh to focus squarely on solving this problem. For this reason, in the summer of 2019, Bill Faloon and I founded the Vitality in Aging Research Group.
The Vitality in Aging (VIA) Research Group seeks to solve this problem and plague of aging by pursuing two separate tracks.
Vitality in Aging Interventions Program: Halt the plague of aging
The plague of aging demands immediate remedial measures, as would any plague. People are dying of aging – tens of thousands per day – and we need to learn how best to keep those alive who are at most immediate risk. For Bill and me and so many others born in the 1950s and 1960s, this goal has deep personal significance: We have elderly parents who, with no antiaging treatments, will not live to see the dramatically effective therapies likely coming in ten to twenty years. And regardless of whether it’s a parent, aunt, uncle, grandparent, or neighbor, all of us should seek to keep our elders alive and well: they are the living, breathing bearers of the cross-general wisdom our society so desperately needs.
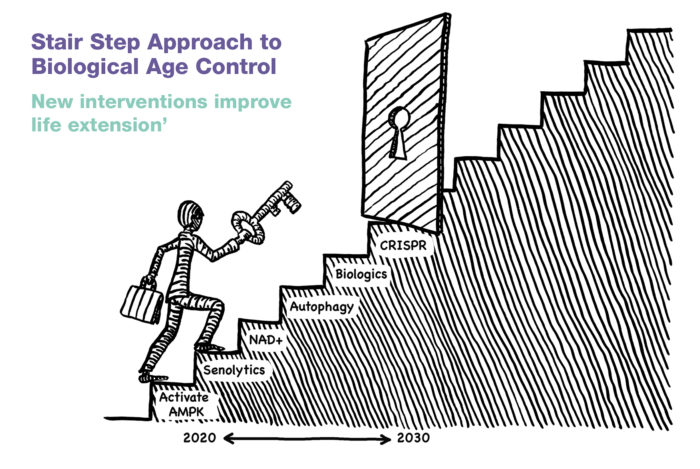
In order to identify, optimize, and test the safety of treatments that could be made available today for those who most need them, VIA created the Interventions Program. This program is designed to bring order to the often-chaotic information with which we are so often presented about how to put into practice the knowledge we already possess about promising interventions. Which of these interventions should one undergo first? How do we arrive at the optimal protocol? How do we identify and mitigate risks?
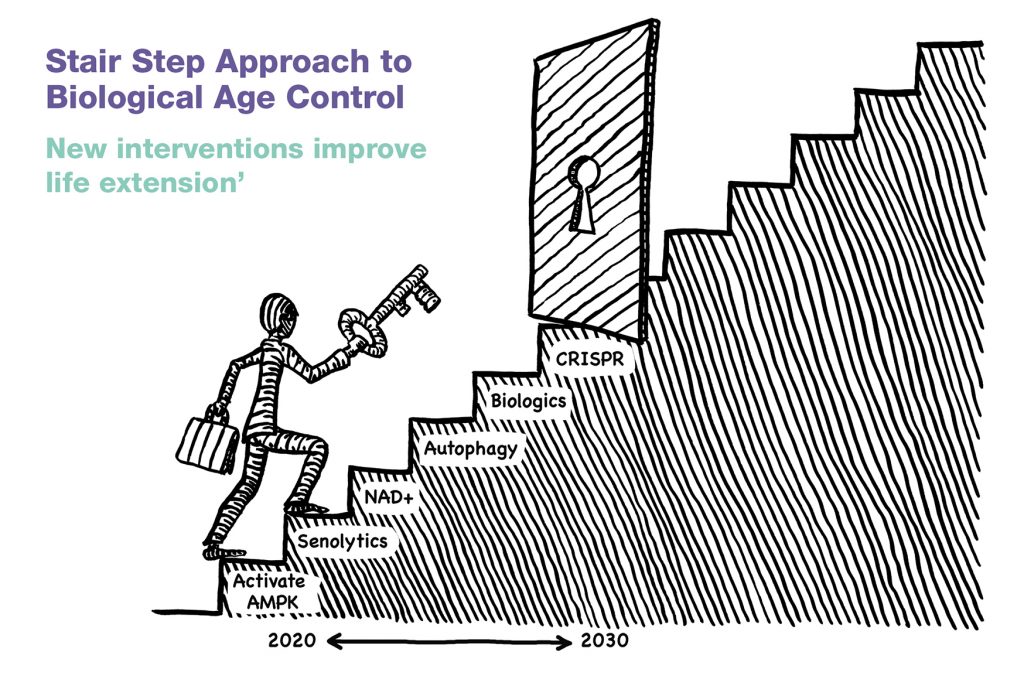
The first trial that we created under the Interventions Program is the VIA Interventions Trial. This is a multi-intervention trial seeking to test the safety and efficacy of several putative antiaging treatments with which many of us have already started experimenting. The interventions and schedule of treatment are shown in table 1. The trial is planned to run for 15 months. After the fifteen-month period has elapsed, we will evaluate the results, and either extend the trial, likely adding new interventions, or start with a new set and schedule of interventions. We also intend to run several other trials in the coming years, in order to test promising but mostly neglected individual compounds. For example, does rapamycin really increase autophagy? Or does metformin really improve glucoregulatory markers?
| Betaine |
| Dasatinib |
| Fisetin |
| Glucosamine |
| Gynostemma pentaphyllum |
| Metformin |
| Nicotinamide riboside |
| Pterostilbene |
| Quercetin |
| Rapamycin |
In the life-extension community, the practice of geriatrics is often denigrated as bandaidery, (too little too late). But geriatrics in some cases might keep some of our elders alive long enough for them to be able to benefit from future interventions that address the root causes of aging, something that geriatrics often fails to address. In many ways, our Interventions Program is a kind of ‘advanced geriatrics.’ We seek to make this program so advanced that anyone who has aged at all – even people in their twenties – can benefit from the findings the program generates. After all, all adults are aging, and all of us need treatment.
Vitality in Aging longitudinal study: Solve the problem of aging
While the plague of aging constitutes an emergency that requires immediate application of whatever measures we have on hand, the problem of aging – understood in the sense of a mathematical puzzle that needs to be solved – requires us to take a step back, or rather a step up, into the realm of basic science.
The current COVID-19 pandemic provides a perfect analogy: humanity must use what we have at hand; whether that be physical distancing, sanitizers, masks, vitamin C infusions, colloidal silver, vitamin D3, mushroom extracts, oregano oil and antiviral drugs etc., to save lives that are under threat now from the plague, but we can’t be penny-wise and pound-foolish: basic science must also be prioritized in order to find a cure along with highly effective preventive measures, such as a vaccine, in order to have a more comprehensive, long-lasting solution to the problem of COVID-19.
To solve the problem of aging, we have adopted a second research track: the creation of a large, observational study designed to understand aging in sufficient detail that we will have a biological roadmap to the development or discovery of highly effective treatments, treatments that will stop and ultimately reverse all aspects of aging. The VIA Longitudinal Study is thus designed in the spirit not of geriatrics, but of gerontology: What is the ultimate logic (logos) of aging body (geron)?
Bill Faloon, our colleague Dr. James P. Watson, and I were all inspired by the achievements of the Framingham Heart Study, and reasoned that a study of aging that followed the Framingham model might ultimately achieve similarly powerful results in the realm of the biology of aging. Let us review the Framingham Heart Study in order to see what an observational can achieve.
The Framingham Heart Study: An exemplary search for the root causes of a serious medical problem
In much the same way that, today, most people regard death as a natural and unavoidable consequence of aging, people living in the first half of the twentieth century regarded heart disease and high blood pressure as ‘normal’ consequences of aging. It was only with the untimely demise of a cherished, war-time American President that this attitude began to change.
By the early 1940s, half of all deaths in the US were caused by cardiovascular disease. Yet at that time, few of the risk factors for cardiovascular deaths were known, so heart disease was regarded as an unfortunate, but inevitable consequence of aging. In the 1940s, even the President of the United States was suffering from untreated hypertension. As early as 1932, before he became President, Franklin D. Roosevelt’s blood pressure was measured at 140/100 mm Hg. Yet his doctors ignored this, since 140/100 was then considered to be ‘normal blood pressure’ for a man of his age. In April 1945, when his blood pressure reached 300/190, the President died of a cerebral hemorrhage. He was only 63, and his death was completely preventable.
The president’s premature death made an indelible impression on the American public and prompted the medical community to question the long-standing conventional wisdom that hypertension did not need to be treated. In 1948, largely as an outcome of FDR’s death, President Harry Truman signed into law the National Heart Act, which included funding for a 20-year epidemiological study of hypertension and heart disease. $500,000 (that’s around $5,000,000 in 2020 Dollars) in Federal grant money was made available for this study and awarded to the US Public Health Service.
The town of Framingham, Massachusetts, was chosen as the location for this epidemiological study of hypertension and heart disease. This one study has yielded more scientific discoveries about heart disease than any other research study in history.
In the two decades following the death of President Roosevelt, the Framingham researchers proved that many of the commonly accepted medical beliefs from the 1940s were erroneous. They showed that in patients with blood pressure over 165/95 mm Hg, there was a four-fold increase in coronary heart disease. They also showed the direct link between hypertension and stroke, as well as between hypertension and heart failure. Research from the Framingham Heart Study was also the key to establishing the link between diabetes and cardiovascular disease. Framingham researchers were also one of the earliest groups to show the cardioprotective value of high-density lipoprotein (HDL).
Researchers from the Framingham Heart Study were also among the earliest to show that obesity was an independent risk factor (from diabetes, hypertension, etc.) for cardiovascular disease. Research at the Framingham Heart Study also provided some of the earliest evidence for the link between atrial fibrillation and stroke risk. The success of the research made it clear that there was no reason to stop at the twenty-year mark. Indeed, the study continues to this day! Today, 70 years after the Framingham Heart Study was launched, researchers are still discovering new details about hypertension and heart disease. Over 3,000 peer-reviewed scientific papers have been published based on the data gathered by the Framingham Heart Study.
Just as the Framingham researchers observed the subjects in their study long enough and carefully enough to glean new details about heart disease and hypertension, we intend to observe a large cohort of people over many years to unearth new details about biological aging. These details will then be used to guide our thinking about the development of better treatments for aging.
Measuring biological age
The Framingham researchers observed participants’ habits and lifestyle choices and then observed which ones were correlated with markers that they hypothesized are predictive of health outcomes, (cholesterol, blood pressure and so on), as well as which ones were correlated directly with the health outcomes themselves – including the outcome that is of the greatest interest and concern to most of us: mortality.
The outcome – or a particular-measure that is a proxy for the outcome – of a scientific study is often referred to as the endpoint of the study. This term takes on a particularly grim meaning in a study focused on aging itself: In a study of aging, the most relevant scientific endpoint is precisely the point at which life ends: death. Yet we do not want to rely solely on this objective, scientifically powerful, yet tragic measure: each death observed would end up twinning scientific utility with an ultimate sign of scientific failure, the failure to have solved aging. If our work and that of other researchers proceeds as quickly as we hope it will, there will thankfully be too few deaths within a reasonable timeframe for this ultimate endpoint to have statistical relevance.
If we want to observe lifestyle and health choices to see how they correlate with a deceleration of the aging process, yet don’t want to wait decades to be able to have a large, statistically significant body count from among those we’d love to keep alive and well, we must have scientific endpoints other than the point at which life ends. Yet we need endpoints with objectivity. This requires accurate and precise measures of biological, or functional age.
We almost always know to the day (and sometimes even the hour) when someone will die. The ideal measure of biological age would be just as precise. For example, let us say that someone who is chronologically exactly 50 years old (1) tries weekly rapamycin for 60 calendar days, then (2) we measure their biological age after the rapamycin treatment, and (3) see that the biological age is 50 years and 49 days, even though his calendar age is now 50 years and 60 days. So imagine this measure is indeed accurate to within one day. Such a precise and accurate measure of biological age would utterly transform all clinical research into understanding aging, including of course not just observational studies, but intervention studies as well. Trials could be far shorter and have far fewer subjects. This would mean, of course, that the money and other resources needed to conduct these trials would be far more modest than that which is needed today. There would be an explosion of clinical trials for all the promising antiaging treatments that many of us have been learning about and are eager to try.
A measure of biological age that has day-length precision is of course an unrealistic goal for the foreseeable future. But any improvements in the suite of tests of biological age that research has at its disposal will accelerate the achievement of effective antiaging treatments. A significant goal of the Vitality in Aging Longitudinal Study is thus to develop better measures of biological age. These improved measures will be needed in order to solve aging as quickly as possible, before more of us perish.
But without the objective touchstone of actual longevity achieved, how can an objective test of biological age be developed? Why would the connections drawn between biomarkers and biological age not be simply a castle in the sky – tetherless and groundless?
The answer, in short, is that biomarkers of biological age can have objectivity by some old-school measures of functional age, along with some biostatistical wizardry. The traditional measures of functional age include tests such as grip strength, hearing threshold, the six-minute walk test, and so on. Even reports of aches and pains can be extremely useful.
For example, we know that osteoarthritis tends to increase with age. If an intervention improves symptoms of osteoarthritis, we might be able to conclude it has slowed aging. Depending on the intervention, it may be that the effect is local, and won’t affect whole organismal aging. A conventional knee replacement, for example, is unlikely to slow aging. But when we have reason to believe an intervention has systemic effects, and when we have enough effects that we can examine – as well as enough interventions – we can begin to get a sense both of whether an intervention is having a systemic effect, as well as how strong the effect is. If we give someone a treatment that we know reduces inflammation globally, and we see improvements in cognition, improvements in autoimmunity, along with improvements in joint pain, then we might be able to conclude it is having a systemic effect on aging.
In seeking to develop new measures of biological age, we will be standing on the shoulders of a veritable army of giants. The phenomenon of inflammation provides one of many examples: Without the development of the theory of ‘inflammaging’ – the idea that increasing systemic inflammation is part of the aging process – we would not even know to look at anti-inflammatory interventions as potential modifiers of biological age.
Our targeted enrollment drives and unique cohort
The Framingham Heart Study sought to examine a representative sample of Americans. Likewise, the Vitality in Aging Longitudinal Study seeks to enroll a diverse and representative group of people. Yet there is one way in which participants will, on average, be decidedly non-representative. Because those connected to Vitality in Aging Research Group are generally keenly interested in health and longevity, the people most likely to hear about our studies and enroll in them are deeply committed to the project of living a long, healthy life. In the Framingham cohorts, the proportion of people who exercise regularly and eat well is small, precisely because these individuals fairly accurately represent the regrettably small proportion of those in the US who engage in healthy behaviors. The proportion of those who seek out antiaging treatments is smaller still. In our cohort, we expect to see many people trying even exotic treatments.
Moreover, because the participants in our trials believe so strongly in the goal of the research, they are highly motivated to provide us with meticulous information about their health and undergo frequent testing. In this way, we expect our data will be unusually detailed and robust.
In fact, our very first enrollment drive, at RAADfest in October 2019, serves as an example of the enthusiasm of our research participants, which of course delighted us (even overwhelmed) us.
RAADfest, as many readers of Aging Matters™ are aware, is a large event put on by the Coalition for Radical Life Extension every autumn in the Southwestern United States, (last year and this year the site is Las Vegas). The Coalition generously offered us help in setting up our own ‘clinic’ in an area of the exhibit hall known as RAADclinic. Given the fee for joining the study (around $500), the amount of time it would take to enroll, and the desire of event attendees not to miss the exciting presentations on the main stage, we thought we might get 50–70 enrollees. We planned for 100 just to be safe. At the end of the conference, we had enrolled 260, and had to turn people away because time ran out. We were thrilled!
We had another enrollment drive at People Unlimited in Arizona a month later, where we enrolled another 60 people. Even now, during the COVID-19 pandemic, we have people contacting us all the time wanting to know when an enrollment drive will be taking place near them.
Reaching for thousands of participants, or: Science in the time of COVID-19
The enthusiasm of our participants will help propel our study forward and yield meaningful results quickly. But we naturally want to make our study open to everyone, including those who, whatever their level of interest in the goals of the study may be, might simply not have time to commit to a rigorous schedule of testing.
We thus decided to create multiple levels of engagement in the study. We will of course encourage everyone to take as many of the tests as possible that we will make available: The more data we can gather, the better. We will be offering cognitive testing, various tests of strength and endurance, whole genome sequencing, DNA methylation testing, numerous blood-based biomarkers, and more. But some of these tests will be optional. The only mandatory steps for participants in the trial – after the completion of the informed consent – are an online medical history and questionnaire, and a blood draw for the Age Management Panel, which is a collection of blood tests available from Life Extension® that was designed especially for the Vitality in Aging studies. The Age Management Panel includes so many markers of health that, armed with these biomarkers and the health questionnaires alone, we expect to be able to draw powerful scientific conclusions about aging.
In this strange historical moment, where we find ourselves in the midst of a global crisis the likes of which has not been seen for generations, the ability to participate in our longitudinal study with minimal physical interaction with others will enable our study to move forward without undue delay. Aside from one trip to a LabCorp blood draw center, staffed by healthcare professionals who know how to keep their customers safe, participants can take part in the trial without leaving their home.
Conclusion
As time goes on, our longitudinal study and intervention trials will feed results into each other. This will enable each to be refined by the other. Methods of solving the plague of aging with targeted interventions we have at hand now will be refined by the results of careful observations of the outcomes of lifestyle and treatment choices, and the outcomes of targeted intervention trials will help refine the nature of the measurements observed in the longitudinal study.
Ideally the gap between gerontology and geriatrics will be closed: An understanding (logos) of the aging body (geron) can be developed that is detailed enough that the doctor who treats the aging body, the geriatrician, knows both how to prevent aging in those who are young, and reverse aging in those who are aged. That is the guiding vision of Vitality in Aging Research Group.