Reducing Toxic Heavy Metals
May 3rd, 2022By Will Block
Metals such as arsenic, cadmium, chromium, lead, and mercury have no beneficial role in human biological functions.[i] Moreover, they and other heavy metals — those with relatively high densities, atomic weights, or atomic numbers — contribute to noncommunicable chronic diseases. These metals have been increased in our bodies by industrial and anthropogenic activities, as well as modern industrialization. The industrial activities of the last century have caused massive increases in human exposure to toxic heavy metals (THM).[ii]
Nevertheless, some orthodox physicians deride claims of any benefits for various therapies, belittling the concerns of health-conscious people worried about potential adverse effects from heavy metals (HM).
DANGEROUS AT ANY LEVEL
It is now clear that low levels of HMs—even at levels that were once considered “safe”—are, in fact, highly dangerous. Evidence of the toxic effects of these metals as they accumulate in the body over time is very strong. Scientists have conscientiously sought methods to remove them from the body. That process is called chelation.
CHELATION GRAB
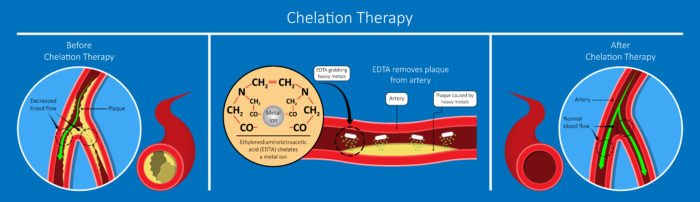
Chelation means “to grab” or “to bind.” When EDTA (ethylenediaminetetraacetic acid), a leading chelator, is inside the veins, it “grabs” heavy metals and helps remove them from the body. EDTA is a synthetic amino acid food preservative that has been used for nearly 60 years to clinically treat heavy metal toxicity and chronic degenerative diseases—especially, cardiovascular disease and cancer.
Nonetheless, as already stated, some scientists believe that except as a treatment for lead poisoning, chelation therapy is controversial and unproved. This is due to the failure of the Center for Disease Control to define other illnesses as caused by HMs.
POISONING RESTRICTION
While novel drug targets for chronic disease are eagerly searched for, potentially helpful agents that aid in detoxification of toxic elements have largely been restricted to covert acute poisoning. As a natural process, chelation occurs when multiple coordination bonds between organic molecules and metals are broken. This is very common in the body and at the heart of enzymes with metal cofactors such as copper or zinc.
Also, the peptides glutathione and metallothionein chelate both essential and toxic elements as they are sequestered, transported, and excreted. Enhancing natural chelation detoxification pathways, as well as use of pharmaceutical chelators against HMs have been reviewed.[iii]
SUBTLE SIGNS OF HEAVY METAL TOXICITY
While signs of acute toxicity are easier to spot (severe cramping, vertigo, vomiting, a green color in feces, difficulty breathing, impaired motor and cognitive skills, etc.), more subtle signs that you need to detox heavy metals are:
- fatigue
- headaches
- acne
- poor digestion/bloating/gas
- compromised ability to digest fats
- female problems (hormones, infertility, preeclampsia)
- excess sweating
- gaining weight just around the waist
- severe food cravings
- middle-of-the-night insomnia
- aching joints
- mood swings
- and the list goes on …
Left unchecked, HMs can cause not only misery but serious disease including Alzheimer’s, dementia, multiple sclerosis, Parkinson’s, and cancer. As the 2013 article in Scientific World Journal explains (already cited):
Historical adverse outcomes with chelators, lessons learned in the art of using them, and successes using chelation to ameliorate renal, cardiovascular, and neurological conditions highlight the need for renewed attention to simple, safe, inexpensive interventions that offer potential to stem the tide of debilitating, expensive chronic disease.
ORALLY-ADMINISTERED DMSA
DMSA (dimercaptosuccinic acid) is a sulfhydryl-containing, water-soluble, non-toxic, orally administered metal chelator which has been in use as an antidote to heavy metal toxicity since the 1950s. More recent clinical use and research substantiates this compound’s efficacy and safety, and establishes it as the premier metal chelation compound, based on oral dosing, urinary excretion, and safety characteristics compared to other chelating substances. DMSA’s water-solubility, oral dosing, large therapeutic window, and low toxicity make it the chelator of choice for many applications.
Approximately 20% of orally administered DMSA is absorbed from the gastrointestinal tract, although this is two-four times the percentage of EDTA. It is believed that one of the sulfhydryls in DMSA binds to a cysteine molecule on albumin, leaving the other sulfhydryls to chelate metals.
In addition to mercury, lead, arsenic, cadmium, aluminum, nickel, uranium, thallium, there are other definitions that include manganese, iron, lithium, zinc, and calcium (yes, under certain conditions very high levels of even essential minerals can become dangerous). Most of these can be taken orally, some regularly, some occasionally.
HEAVY METALS IN SOME FOODS
Where do heavy metals come from? Here are some of the heavy metals causing toxicity in our modern environment and their common sources:
- Lead (auto exhaust, root canals, building materials, water, some teas).
- Mercury (dental fillings, vaccines, contact lens solution, seafood).
- Cadmium (cigarettes, batteries, hydrogenated oils, coffee).
- Arsenic (conventional poultry and eggs).
- Aluminum (deodorant, vaccines, cookware, some teas).
- Thallium (added to gasoline).
- Bismuth (makeup, medicines).
The list certainly goes on, but these are a few of the key players.
MIND YOUR SOURCES
When you want to limit heavy metals exposure you cut down on meats and seafood. Of those that you do eat, make sure you use reliable sources. Also, use holistic dentistry, natural deodorants, and beauty products, and avoid hydrogenated oils. Unfortunately, we may not have as much control over other things on the list.
FOODS THAT REMOVE HMs
What foods can help remove heavy metals from the body? As you’ll learn more about below, foods to include in a heavy metal detox include leafy green veggies, other non-starchy veggies, herbs, spices, algae and other superfoods, and bone broth.
LEAD INCREASES VASCULAR DISEASE AND OVERALL MORTALITY
Acute lead poisoning (short-term, high exposure) causes symptoms of abdominal pain or “lead colic,” cognitive deficits, peripheral neuropathy, arthralgias, decreased libido and anemia. Research shows that it can be diagnosed by a characteristic “lead line” at the junction of the teeth and gums, and by high blood lead levels (over 80 micrograms per deciliter).[iv] (Figure 1)
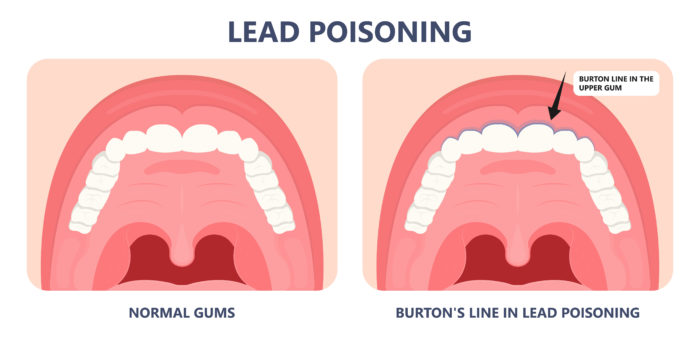
Figure 1: A bluish line in the gum line is one sign of an over exposure to lead. Called the ‘Burton line’ after its discovery by Henry Burton in 1840.
Yet, the effects of chronic exposure to low levels of lead are not easy to determine. Long-term exposure to low levels of lead may result in the gradual accumulation of lead and the development of a number of disorders and diseases, including learning and behavior problems, cardiovascular and kidney diseases, decreased fertility, hypertension and cancer.
EFFECTS OF LOW LEVELS OF LEAD
To determine the effects of chronic exposure to low levels of lead, data from the massive Third National Health and Nutrition Examination Survey (NHANES-III) was explored.[v] NHANES data is a stratified, multistage probability sample of the civilian non-institutionalized individuals within the United States.
This study demonstrates the potential dangers of social and environmental exposures to liver health. No level of lead exposure is safe, and even very low levels of exposure may significantly harm the health of individuals.
Lead exposure may come about due to exposure from lead-contaminated paint, water, jewelry, candy, soil, and dust.
THE ROLE OF CHELATION THERAPY
Chelation therapy provides benefits by reducing the body burden of HMs, resulting in improved physiological functioning and better health. The two most widely used oral chelating agents are EDTA and DMSA.
DMSA—A CHELATOR SINCE THE 1950s
DMSA (meso-2,-3-dimercaptosuccinic acid) is a sulfhydryl-containing, water-soluble, non-toxic, orally administered metal chelator that has been in use as an antidote to heavy metal toxicity since the 1950s.
DMSA is the premier oral metal chelator for mercury and is effective for other heavy metals as well. DMSA’s water-solubility, oral dosing, large therapeutic window and low toxicity make it the chelator of choice for many applications.
LEAD INCREASES CERTAIN CANCERS AND OVERALL MORTALITY
Lead poisoning has long been recognized as a health hazard. This HM has been historically used in a number of industrial processes. These include the manufacture of batteries, paints, and as an additive in gasoline.
However, the effects of chronic exposure to low levels of lead are more difficult to determine. Long-term exposure to low levels of lead may result in the gradual accumulation of lead and the development of a number of disorders and diseases, including learning and behavior problems, cardiovascular and kidney diseases, decreased fertility, hypertension and cancer. The effects of chronic exposure to low levels of lead is a concern.
NO SAFE LEVEL OF LEAD
There is no safe level of lead. Lead at any level contributes to increased disease-related mortality—especially from heart disease and cancer. Lead is still found in millions of pre-1940s homes. Lead toxicity impairs calcium uptake and utilization and interferes with calcium-facilitated cellular metabolism.
Lead is especially toxic to the central nervous system, as evidenced by its harmful effects on mental development and intelligence in children, who are especially susceptible to lead’s deadly effects. For example, behavioral disorders such as attention deficit disorder (ADHD) have been attributed to lead exposure.
MERCURY AND CARDIOVASCULAR DISEASE
Until recently, the notion of treating heart disease with chelation therapy—one of the mechanisms of which is to remove heavy metals—was scorned by the medical establishment. Nevertheless, alternative therapy has overruled that idea.
In several recent studies, mercury has been found to be connected to CVD. In one, a systematic review of published studies and a meta-analysis of the results to examine the associations between chronic Hg exposure and CVD outcomes was run.[vi] In this study, mercury was found to be associated with all-cause mortality and fatal/nonfatal ischemic heart disease.
Mercury compounds also promote platelet aggregability and blood coagulability.[vii] They also inhibit endothelial-cell formation and migration and affect apoptosis and the inflammatory response.
Increased rates of cardiovascular disease were found in mercury-exposed workers, and mercury levels in hair predicted the progression of carotid atherosclerosis in a longitudinal study. An article in the 2002 New England Journal of Medicine, found that mercury levels were directly associated with the risk of myocardial infarction (heart attacks), and that this partially offset the protective effects of DHA derived from eating fish.[viii]
They editorialized: “The notion that methylmercury contributes to cardiovascular disease is certainly a testable hypothesis and one that warrants further testing.” Continuing: “Mercury, fish oils, and the risks of myocardial infarction… Mercury may promote atherosclerosis and hence increase the risk of myocardial infarction in several ways. Mercury promotes the production of free radicals … and may bind selenium [so that it] cannot serve as a cofactor for glutathione peroxidase. Mercury may … inactivate the antioxidant properties of glutathione, catalase, and superoxide dismutase.”
The New England Journal of Medicine went on: “The notion that methylmercury contributes to cardiovascular disease is certainly a testable hypothesis and one that warrants further testing.”
Fish consumption is directly associated with methylmercury levels in blood and hair.12,13 Mercury in dental amalgams is probably the major source of inorganic mercury exposure in humans.14 The most commonly used dental amalgam material contains approximately 50% liquid metallic mercury.
Thus, amalgam preparation and placement results in mercury vapor exposure for the patient, dentist and technician. Mercury vapor continues to be released as the patient chews, brushes, or drinks hot beverages, after which it is inhaled into the lungs and enters the bloodstream.
Studies have shown a direct correlation between the number of amalgam fillings and mercury concentration in blood and urine. Amalgam removal reduces blood-mercury levels.
DMSA treatment results in the greatest urinary excretion of mercury, compared to other heavy metal chelators, as well as being the most effective at removing mercury from the blood, liver, brain, spleen, lungs, large intestine, skeletal muscle and bone.
Mercury excretion is greatest in the first eight to 24 hours after ingestion of DMSA. In animal studies, DMSA was the most efficient chelator for brain mercury, removing two-thirds of the brain mercury deposits.
SAFETY OF DMSA
DMSA is very safe, and usually causes few side effects. Some may experience slight gastrointestinal distress or itching, when higher doses are used. As with any chelating agent, DMSA can cause deficiencies of copper, manganese, molybdenum, and zinc, especially if they are not replaced by supplementation. DMSA doesn’t directly bind magnesium, cysteine, or glutathione, but heavy metal detoxification can result in depletion of these nutrients as well.
Likewise, EDTA can also remove zinc and selenium, and therefore whilst chelating those heavy metals it is always prudent to supplement with a multi-mineral.
DOSAGE RECOMMENDATIONS
Dosage recommendations for DMSA are quite different depending on your source. In Physicians’ Desk Reference and other conventional medical publications, the recommendation is 10 mg per kg every eight hours for five days; then reduce the dose to twice daily for two more weeks, off for two weeks, and repeat as necessary.
As far as EDTA is concerned, the doses are often in the range of 500 mg to 1000 mg daily taken over several weeks and repeated as necessary.
Of course, it is always best to do a before and after heavy metal test, to see what is afflicting you and how it is being reduced.
Note: Heavy metal detoxification is a long-term process, as the heavy metals in the body compartments are in a constant state of equilibrium.
References
[i] Sears M. Chelation: Harnessing and Enhancing Heavy Metal Detoxification — A Review. Scientific World Journal 2013 Apr 18; 2013:219840.
2 Balali-Mood M, Naseri K, Tahergorabi Z, et al. Toxic Mechanisms of Five Heavy Metals: Mercury, Lead, Chromium, Cadmium, and Arsenic. Front Pharmacol. 2021; 12:643972
[iii] Rahman Z, Singh VP. The relative impact of toxic heavy metals (THMs) (arsenic (As), cadmium (Cd), chromium (Cr)(VI), mercury (Hg), and lead (Pb)) on the total environment: an overview. Environ Monit Assess. 2019 Jun 8;191(7):419.
[iv] Marsden PA. Increased lead burden—Cause or consequence of chronic renal insufficiency? New England J Med 2003, 4:345-6.
[v] Obeng-Gyasi E. Cumulative effects of low-level lead exposure and chronic physiological stress on hepatic dysfunction-a preliminary study. Med Sci (Basel) 2020 Aug 5;8(3):30.
[vi] Hu XF, Lowe M, Chan HM. Mercury exposure, cardiovascular disease, and mortality: A systematic review and dose-response meta-analysis. Environ Res. 2021 Feb; 193:110538.
[vii] Lohren H, Bornhorst J, Galla HJ, Schwerdtle T. The blood-cerebrospinal fluid barrier–first evidence for an active transport of organic mercury compounds out of the brain. Metallomics. 2015 Oct;7(10):1420-30. doi: 10.1039/c5mt00171d. Epub 2015 Aug 12. PMID: 26267314.
[viii] Bolger PM, Schwetz BA. Mercury and Health, New England J Med 2002, 347:22, 1735-6.M