A healthy mouth for a healthy body
April 20th, 2021By Brian Halvorsen, BDS, LDS, RCS
Dr. Brian Halvorsen has been practising dentistry for over forty years and has provided holistic and preventative dental care for 35 years. His book ‘great teeth for life’ explains his views on holistic and preventative health and forms a dental education for every generation. Based in London, England, Dr. Halvorsen provides holistic integrated advice and treatments under the slogan that; “a healthy toxic free mouth contributes to a healthy body and mind.”
As a dentist I have been extremely active in general wellbeing, antiaging and detoxification. In over 45 years of General Practice, most with a holistic and preventative approach, I have cared for thousands of patients that have joined my Practice as children and have themselves become parents and even grandparents! I soon realised how general health was often related to dental health. Poor diet, (I also include smoking, narcotics, and alcohol) and negative life stress contributes to gum disease and tooth decay by reducing a person’s immune system and triggering inflammatory responses.
Over many years, through observations, careful monitoring, and specific research, I noted the relationship between good dental health and general health.
So, I ask these questions; “can good mouth health improve our overall health and wellbeing? Can poor oral health contribute to greater disease in our body and mind?” And I answer both these questions with an unequivocal-
“Yes!”
Many well respected and World-renowned health practitioners and researchers claim that between 50% and 80% of all disease originates from the mouth. If this seems incredible, in a recent interview with one of the World’s most esteemed consultant periodontists, Professor Iain Chapple; he disclosed, that in countries where healthcare is provided privately, when people over the age of 50 years have excellent oral health, their medical bills are often reduced by as much as 40%! (1)
The question becomes; “If oral health does play such an important role in our overall health and well-being, then what are the biological mechanisms and processes involved?’’
Background
A healthy body is covered in an unbroken protective ‘skin’ which prevents unwanted chemicals entering our bloodstream and tissues.
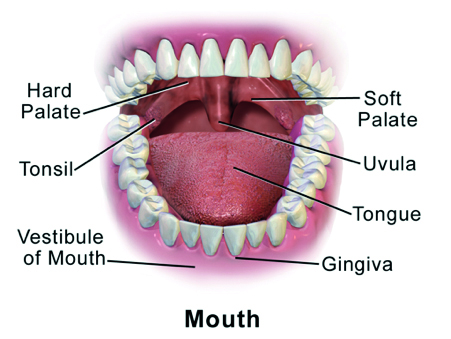
In the mouth, our teeth have grown through this ‘skin.’ There is a join where part of the tooth structure stands above the jawbone/ gum. The gap between the root and the gum is the gingival crevice and is referred to by dental professionals as the ‘pocket’. If the health and integrity of the junction between root, gum and jawbone becomes diseased, systemic inflammation occurs.
In a healthy mouth, with healthy gums, the seal around the tooth is mainly unbroken. Even so, in healthy mouths, there will always be areas where small amounts of inflammation can occur (known as localised gingivitis).
Where there is gingivitis, the seal is broken, allowing entry to the bloodstream of inflammatory products, such as chemicals from food, bacteria, viruses, yeasts, toxins etc. In mild gum disease the body’s defences [Immune system] can cope with these inflammatory invaders, quickly and effectively, so these bugs can be mopped up and are not allowed to spread around the body.
Severe, and prolonged gum disease [periodontitis] often leads to chronic inflammation of our entire body. This has serious health implications. Current evidence-based research implicates gum disease with increased risk of Cardio- vascular disease, type-2 Diabetes, many Cancers, sepsis, neuro- degenerative disease, such as Alzheimer’s and an exceptionally long list of inflammatory diseases including rheumatoid and osteo arthritis. (2)

Oral bacteria are subject to a great deal of research. Already certain strains have been discovered that may impact Alzheimer’s, specifically Porphyromonas gingivalis, the bacteria present in the most serious form of gum disease. Researchers found this bacterium can travel from the mouth to the brain, creating toxins called gingipains that cause damage to human proteins and destroy brain cells and nerves, and is more common in the brains of people with Alzheimer’s than those without.
Porphyromonas gingivalis is present in many people but, like other types of bacteria, it becomes a problem when it overgrows. This is how periodontitis happens, with inflamed, eroding, bleeding gums, and just chewing can spread bugs into the bloodstream.
If somebody has a genetic predisposition to Alzheimer’s, then good dental health may be a part of a preventative regime. Same goes for those with rheumatoid arthritis, since Porphyromonas gingivalis may also play a role in the progression of that disease as well. (6)
And this is just one type of bacteria! There are thousands upon thousands of species present in the human mouth and consequently the body, impacting all areas of it.
When I was an undergraduate over 40 years ago, dental students were taught, and still are, that another bacterial strain, Streptococcus mutans can escape from the mouth and infect faulty heart valves, leading to a profoundly serious infection – sub-acute bacterial endocarditis [SBE]. If not treated appropriately SBE is likely to be fatal.
This is one of the reasons why dentists ask, in detail, about your medical history. It could be stated that first line of whole-body preventative health starts with good oral hygiene and a healthy mouth.
The connection between the mouth, gut, and brain
Again, another area of research is the microbiome and human health. Gut bacteria can influence neurotransmitter activity and neurodegenerative diseases like Alzheimer’s and Parkinson’s and the source of gut bacteria and its ecology comes from the mouth. Although nutrition has a huge influence on gut microbiome, the mouth is where digestion starts, and where food influences both growth and composition of oral microbes. Reproduction rate of oral bugs is phenomenal. It has been estimated that over 3 billion bugs grow in a 24-hour period and are swallowed into the digestive system thus having a huge influence on the health and ecology of the gut microbiome.
At the root of the problem [excuse the pun] is the person’s immune system. When bugs, toxins and foreign bodies invade our body via the oral tissues, especially the gums, our white cells are stimulated (it is an inflammatory response).
Even brushing our teeth and gums in a healthy mouth will push some bugs etc. into the bloodstream. Immuno-compromised people such as uncontrolled diabetes, cancer patients on chemotherapy and those suffering long-term debilitating illnesses may find difficulty coping with a mild attack of gingivitis. Conversely, people with a compromised immune system have greater difficulty maintaining a healthy mouth as healing response is reduced. The health of the body cannot be separated from the health of the mouth and vice versa.
Therefore, it is vitally important to see a dentist and /or hygienist if you have general health problems. Patients often ask why there is so much emphasis on giving medical, lifestyle, nutritional and phycological history before a dental examination/ consultation. By taking a holistic approach many seemingly unrelated health issues can be influenced by mouth health and vice versa.
Back in the mouth
If the gums bleed occasionally, especially on brushing, please do not believe the adverts suggesting that your teeth will fall out next week! Mild gingivitis/ bleeding is reversible; but do see your dentist/hygienist. In most cases the number of bugs entering the bloodstream is likely to be comparatively small and are likely to be mopped up immediately. Again, following a cleaning with a dental hygienist, a higher number of bugs will enter the bloodstream [transient bacteraemia].
A patient who is in ‘generally good health’ i.e. with a non-compromised immune system, should be able to prevent pathogens spreading to other parts of the body, following routine oral hygiene procedures. Always check with the dentist/hygienist on the risk/benefit of any clinical treatment.
With the reducing effectiveness of antimicrobials, it is essential to maintain good oral health. Sepsis kills thousands, and there has been little research into identifying where these highly toxic bugs originated. To me, the mouth would appear to be high on the suspect list of sites of origin.
In ecological terms, a diseased mouth with gum disease, is a mouth with a predominance of pathogenic [disease causing] bacteria.
Prevention
Given the undisputed relationship between maintaining a healthy oral environment and the effect on overall good health, are there any regimes that can ensure long term mouth health and optimising overall health and wellbeing?
Nutrition
The mouth is the portal for most of our nutrition and is the initial and important part of our digestion.
Sugar, refined carbohydrates, and most over processed food and drink we know will lead to inflammation and disease processes. Most of the dental profession relate this diet to increased risk of tooth decay, but holistically, a poor diet has far more serious consequences for increasing the risk of gum disease and the consequential effects on overall health.
The research to find if a ‘healthy diet’ can improve gum health is scant. Woelber JP et al., has shown diet can improve periodontal health in a paper; ‘An oral health optimised diet can reduce gingival and periodontal inflammation in humans – a randomised control study’. (7)
As Hippocrates, the father of medicine famously said; “Let food be thy medicine and medicine be thy food.’’
Comment
Can you believe that such an obvious relationship between diet and gum health has not been extensively investigated? An obvious example: Early signs of Scurvy, a clinical lack of Vitamin C, is swollen bleeding gums! (Whilst working for a large dental corporate body I was told not to discuss with patients the benefits of taking supplements as there was no ‘evidence-based research’ to back up this advice’…)
Essential fatty acids, vitamin D, vitamin K2, Coenzyme Q10, zinc, magnesium and vitamin C have all been shown to improve oral health. (In combatting gum disease, the dose is important to have a therapeutic effect). With our nutrient poor diet, there a strong case to take supplements to improve gum health.
Oral hygiene
Correct mechanical cleaning of teeth and gums, especially the vital junction where gum joins the tooth root/ jawbone [the periodontal membrane] is essential. Remember, this junction still exists where gums may have receded and is where pathogens and toxins can enter directly into the bloodstream.
Spend time with a good dental hygienist / therapist and don’t just have your teeth cleaned but take time to learn how to clean your teeth and gums effectively and efficiently. Remember, it is not the total time spent, it is the effectiveness and efficiency. By seeing the hygienist regularly our oral hygiene technique will improve with time. We are all creatures of habit, and cleaning our teeth is no exception, so maintaining a healthy mouth can become an autonomic habit like driving a car.
Dental ‘cleaning aids’
Get expert advice from your hygienist, i.e., on the types of toothbrushes, floss, interspace cleaners etc. We are all individuals, and our techniques need to be adapted to our individual mouth anatomy.
Regarding toothpaste, in my experience, most of the ‘popular brands’ are much the same, but none address a way of healing/ repairing the vital junction, [periodontal membrane] despite their claims! As with both toothpastes and mouthwashes, most proprietary brands claiming that their ingredients ‘kill’ bugs and are, by definition, altering the ecology of the mouth. In my opinion, leading to unknown systemic effects. Except for ‘oil pulling’ with organic oils such as coconut, I have been reluctant to recommend any of the mainstream toothpastes and mouthwashes.
For many years now, patients have asked me when they can have a new tooth in their mouth grown by stem cells. Although research is ongoing, there appears to be a while to go before it will become clinically available. When I was asked to review a new peptide repair gel and its mouthwash called OralTidePro™, which uses a similar technology, my interest was piqued.
My basic principals with any product before either using or recommending either to myself, my family and patients are as follows:
- ‘First, does it do no harm?’ In my estimation, a product needs not only to be nontoxic, but also eco-friendly.
- ‘Does it maintain a healthy microbiome?’
- ‘Does it work?’
In these respects, OralTidePro™ has no fluoride, no alcohol, no chlorhexidine, and no potassium nitrate and nor does not unbalance the microbiome, plus its list of positive benefits from its regular use is impressive- OralTidePro™:
- Repairs periodontal connective tissue.
- Repairs gingival recession.
- Protects the dentin.
- Consolidates the teeth structure.
- Improves enamel demineralization.
I am possibly a bit ‘old fashioned’; since I have where possible, tried things out on myself and any willing members of my family, (especially dental products and nutritional supplements), and I can therefore report that my wife and I have both used OralTidePro™ mouthwash and the repair gel regularly for over 6 months. We both like the taste and have noticed that our mouths feel healthy.
Being a scientist, as well as a dentist, the proceeding statement is subjective, but together with the scientific data I have seen, along with its lack of known toxins, I recommend OralTidePro™.
OralTidePro™ intensive repair gel, available through our friends at Profound Health: http://bit.ly/IntensiveRepairGel
OralTidePro™ concentrated mouthwash, available through our friends at Profound Health: https://bit.ly/MouthwashPH
References
- UK Health Radio. Interview with Prof Iain Chapple on ‘The Integrated Dentist’ show. 2018 Effect of Periodontal treatment on diabetes – related healthcare costs; a retrospective study Smith et al., BMJ Open diabetes Res Care Oct 2020.
- Microglial response to experimental Periodontitis in a murine model of Alzheimer’s disease. Kantari et al., Science Rep Oct 2020.
- Periodontal Status and microbiological pathogens in patients with Chronic Obstructive Pulmonary Disease & Periodontitis; A case control study, Zhou X, Wang J et al., International Journal of Obstructive Pulmonary Disease 2020.
- Role of Periodontal Therapy in the management of common complex Systemic Diseases. Study by Sabharwal et al., Periodontal 2000 Oct 2018.
- Periodontal Inflammation primes the Innate Systemic Response, Fine N et al., Journal of Dental Research Oct 2020.
- Rheumatoid Arthritis and Pneumonia link to P Gingivalis, Gum bacteria implicated in Alzheimer’s and other Diseases; Science Daily 7/4/2019.
- An Oral Health Optimised Diet can reduce Gingival and Periodontal Inflammation in Humans – A randomised control pilot study, Woelber JP et al., BMC Oral Health 2016.