Melatonin Stops Cancer!
June 4th, 2020By Will Block
A few years ago, Dr. Frank Shallenberger, a Medical Doctor who makes his practice in Carson City, Nevada- and who also holds a doctorate in Natural Medicine (NMD)—was surfing PubMed, the National Library of Medicine’s database. While there, he ran into an animal study showing that melatonin had an extremely curious effect on active cancers. This was so amazing to him that “it blew his mind.”
What the paper showed was that melatonin could stop cancer from growing—provided the amount consumed was high enough and provided it was taken before sleep under light-restricted conditions.
The key author of the revelatory article was none other than Russel J. Reiter, PhD, unquestionably the greatest melatonin animal researcher in the world, with more than 1,383 scientific articles to date (that averages 25 papers per year for 55 years). In the mind-blowing research piece, scientists fed a group of mice cancer-producing adenocarcinoma and what they noticed—using a method of measuring the growth rate of cancer—was that each night the growth rate of cancer slowed down when the lights were turned off.
What they also discovered was that each morning when the power was restored, the growth rate of their cancers resumed. Guided in his personal protocol by Dr. Reiter, Dr. Shallenberger now takes 180 mg every night, about 45 minutes before sleep. He avoids all light, (absolutely no light, except red light) during the night. These effectively represent total blackout conditioning, with no ambient light permitted. There are no side effects. He uses pure melatonin (see below).
Melatonin Is the chemical expression of darkness
Melatonin is produced and released in your pineal gland as a response to darkness. As per Dr. Reiter, melatonin is the chemical expression of darkness. It is immediately suppressed by all light, whatever the color, except red light. Melatonin is not a soporific (it doesn’t produce sleep). That’s the role of darkness. You can take melatonin during the day, as well as at bedtime, without any adverse effect. There no serious side effects. Some patients report sleep disturbances and AM sleepiness, but these are few.
Dr. Walter Pierpaoli, one of the world’s leading clinical melatonin researchers, has successfully used daily dosages ranging from 0.1 to 200 mg. That’s a 2,000-fold difference between the lowest dose and the highest! Studies on mice show that even at astronomical doses of 300 mg per day for two years, there were no side effects.
Sleep Like a Stone
“Remember when you were a kid, when you couldn’t remember anything from the moment you put your head on the pillow until you awoke. That’s what I experience every night,” reports Dr. Shallenberger. “Nothing happened when I took the large amount. I continued to sleep 7 hours a night. It didn’t go to 8 or 9 and I didn’t get sick!” Then he gave the same amount of melatonin to his wife. She responded much as he had and finally, he gave it to his cancer patients, some of whom have nothing to lose. He gave them 60 mg with meals (breakfast, lunch, dinner) and 60 mg at bedtime (240 mg throughout the day). There were no illnesses.
How much melatonin do you take?
[This is a hypothetical conversation between Dr. Reiter (italic) and Dr. Shallenberger.]
How much melatonin should I take?
Dr. R: I’m not a medical doctor; I’m a PhD.
Just between us … How much do you take?
Dr. R: I take 180 mg every night, all at once. One hundred eighty mg is entirely safe … it’s the equivalent of the amount animals are given.
Do you know anyone else who takes this amount?
Dr. R: No researcher I know takes less than 100 mg per day. They take it at night in balance with their circadian rhythm…
Where do you get your melatonin? How do you know it’s good?
Dr. R: I analyze every batch myself. There are lots of problems with other things that show up in it. Tableting can damage it. Heat is a problem also. As is pressure. It’s got to be pure. To a large extent, impurities are why you and other MDs are seeing many problems. With purity requirements met, people who can take only a little (of the un-pure melatonin) can take a lot.
Peak plasma level
The peak plasma level after oral ingestion of melatonin is about 1 hour. At the 180 mg per night dose, high levels are typically sustained throughout melatonin’s half-life, which is 3-4 hours. Melatonin rapidly enters the central nervous system and crosses the blood-brain barrier. Exogenous melatonin does not alter the levels of any other hormones. There is no negative feedback inhibition.
Melatonin activates anti-neoplastic immune reactivity. Direct anti-cancer action: Protects against chemo-radiation damage. On average, the combined results of these studies showed that melatonin greatly reduces the risk of dying. The effects were consistent no matter what dose they used. None of the patients had any significant side effects from the melatonin.
The substantial reduction in risk of death, low adverse events reported, and low costs related to this intervention suggest great potential for melatonin for treating cancer.
A few of the many articles in print- melatonin can halve the spread of cancer in a wide variety of tumors.
For example, it regulates estrogen receptor expression and transactivation, modulates the enzymes involved in the local synthesis of estrogens, and serves to modulate cell cycle and induce apoptosis.
Moreover, for the inhibition of telomerase activity, plus a similar effect on metastasis, there are direct anti-neoplastic effects. Melatonin decreases cell proliferation at low concentrations and at high concentrations, direct cytotoxic effects occur. Melatonin works as a mitochondrial stimulant.
Furthermore, there is stimulation of cell differentiation and induction of apoptosis and anti-angiogenesis activity. Plus, when it is administered in combination with chemotherapy, a synergistic effect has been found in several cancer types.
There is nothing to lose with high dose melatonin
If you want to spend the afternoon (or weekend … or longer) looking at PubMed, there’s plenty of material there. For example, while still on the melatonin’s anti-cancer front:
The first reference to a possible role of pineal gland in the growth and spread of malignant tumors is attributed to Georgiou writing about this in 1929. These authors concluded that something of pineal origin actually stimulated tumor growth. Almost 50 years later, in 1977, Vera Lapin organized the first international workshop in Vienna on the relationship between the pineal gland and cancer: it’s called The Pineal Gland as a New Approach to the Neuroendocrine Control Mechanism in Cancer.
This workshop systematized all the knowledge generated to the date of the workshop and was the stimulus of numerous studies on the role of pineal gland in the etiology and pathogenesis of neoplastic diseases. Its ultimate goal was to identify therapeutic tools useful in the treatment of human cancer. Curiously, contrary to Georgiou’s original proposal, it is now commonly accepted that melatonin, the most relevant pineal secretory product, has oncostatic (cancer stopping) properties on a wide variety of tumors and, especially, in those identified as being hormone dependent.
Suppressing melatonin
Remember that natural endogenous production of melatonin is immediately suppressed by light, even ambient light, especially blue light, but not red light. Therefore, always sleep in a blacked-out bedroom. However, light will not affect melatonin taken exogenously, in other words, as supplements by mouth.
It can be effective for brain cancers
As mentioned, melatonin rapidly crosses the blood-brain barrier and enters the central nervous system. It is thus beneficial for brain issue problems such as brain cancers and Alzheimer’s disease, Parkinson’s disease, and dementia. Melatonin does not alter any other hormones. As such, there is no negative feedback inhibition.
Gatekeeper of the circadian clock
Melatonin is a naturally occurring molecule secreted by the pineal gland and known as the gatekeeper of the circadian clock. Mounting evidence indicates that melatonin, employing multiple and interrelated mechanisms, exhibits a variety of oncostatic properties in a myriad of tumors during different stages of their progression.
Tumor metastases
Tumor metastases, which commonly occur at the late stages of cancer are responsible for many cancer deaths. Metastases lead to the development of secondary tumors distant from a primary site. In reference to melatonin, most investigations have focused on tumor development and progression at the primary site.
Recently, however, interest has shifted toward the role of melatonin on tumor metastases. In a scientific review, 5 the authors highlight current advances in understanding the molecular mechanisms by which melatonin counteracts tumor metastases, including experimental and clinical observations. They place their emphasis on the impact of both cancer and non-neoplastic cells within the tumor microenvironment.
Due to the broad range of melatonin’s actions, the mechanisms underlying its ability to interfere with metastases are numerous. These include modulation of cell-cell and cell-matrix interaction, extracellular matrix remodeling by matrix metalloproteinases, cytoskeleton reorganization, epithelial-mesenchymal transition, and angiogenesis.
Glucose transporters
In another paper, melatonin is shown to be taken up through members of the glucose transporters family and these thus have a central role in the inhibition of cancer.
Glucose concentration and the presence of competitive ligands of GLUT1 affect the concentration of melatonin in cells. As a regulatory mechanism, melatonin reduces the uptake of glucose and modifies the expression of GLUT1 transporter in prostate cancer cells. More importantly, glucose supplementation promotes prostate cancer progression in Transgenic Adenocarcinoma of the Mouse Prostate (TRAMP) mice, while melatonin attenuated glucose-induced tumor progression and prolonged the lifespan of tumor-bearing mice.
But melatonin does not induce sleep
Contrary to what many believe, melatonin doesn’t make you sleepy. For the sake of our cancer conversation, melatonin is secreted by the pineal gland. Light suppresses it. Melatonin sensitizes us to light, and darkness causes us to sleep. Dr. Shallenberger has been taking it for nearly three years, as have many of his patients. Nobody has gotten any adverse effects from melatonin, even at the high levels they are taking.
Endothelin-1 (ET-1) is a peptide that acts as a survival factor in colon cancer, inducing cell proliferation, protecting carcinoma cells from apoptosis, and promoting angiogenesis. 7 The data presented show that melatonin inhibits END-1 mRNA expression, the first step in ET-1 synthesis.
In conclusion, melatonin may be useful in treating colon carcinoma in which the activation of ET-1 plays a role in tumor growth and progression. Almost all cancer cells produce it.
Melatonin exerts pleiotropic, (many sided) anticancer effects against a variety of cancer types. Herein, the authors review the correlation between the disruption of the melatonin rhythm and non-small-cell lung cancer (NSCLC) incidence. They also evaluate the evidence related to the effects of melatonin in inhibiting lung carcinogenesis. A special focus is placed on the cancer-stopping effects of melatonin, including anti-proliferation, induction of apoptosis, inhibition of invasion and metastasis, and enhancement of immunomodulation.
NSCLC is a leading cause of death from cancer worldwide. As an indoleamine discovered in the pineal gland, melatonin exerts pleiotropic anti-cancer effects against a variety of cancer types. Melatonin may be an important anti-cancer drug in the treatment of NSCLC. Herein, this correlation between the disruption of the melatonin rhythm and NSCLC incidence is reviewed; the researchers also evaluate the evidence related to the effects of melatonin in inhibiting lung carcinogenesis.
The best treatment for any disease is not to get it!
Special focus is placed on the anti-cancer effects of melatonin, including anti-proliferation, induction of apoptosis, inhibition of invasion and metastasis, and enhancement of immunomodulation. The researchers strongly suggest the drug synergy of melatonin with radio- or chemotherapy for NSCLC is valuable. The information herein serves as a comprehensive reference for the anti-cancer mechanisms of melatonin against NSCLC.
Darkness, melatonin and cancer
It is suggested that the drug synergy of melatonin with radio or chemotherapy for NSCLC could prove to be useful.
Melatonin is released in response to darkness. The key cause of disease is the disruption of the circadian system. This is not debatable anymore. If you go to PubMed some day and plug in ‘melatonin,’ you’ll find oodles of material to read. If the half-life of melatonin is 3 hours and you take 180 mg about 45 minutes before sleep, you’ll be at the half-way mark about 4 hours later.
The key cause of disease is the disruption of the circadian system
The aforementioned article burrows into melatonin containing over 140 references.3 It is written by Reiter students Mills and Wu. When looking for melatonin articles, be aware that if Reiter’s name is not on these, his students’ names certainly are. This is a great paper to have in your library. In just a few pages it gives you the lowdown on melatonin.
Melatonin for gastrointestinal cancer
In the review titled Melatonin as a Treatment for Gastrointestinal Cancer, the authors first clarify the relationship between the disruption of the melatonin rhythm and gastrointestinal cancer (based on epidemiologic surveys and animal and human studies) and summarize the preventive effect of melatonin on carcinogenesis.8 Thereafter, the mechanisms through which melatonin exerts its anti-gastrointestinal cancer actions are explained, including inhibition of proliferation, invasion, metastasis, and angiogenesis, and promotion of apoptosis and cancer immunity.
Moreover, the paper discussed the drug synergy effects and the role of melatonin receptors involved in the growth-inhibitory effects on gastrointestinal cancer. Altogether, the information compiled here serves as a comprehensive reference for the anti-gastrointestinal cancer actions of melatonin that have been identified to date.
Almost a slam-dunk
For estrogen dominant and testosterone prostate cancers, melatonin is a key. Apoptosis is important too. Melatonin has a direct and an indirect anti-cancer effect. It proves a very pleiotropic effect on cancer. One thing that melatonin is very effective for is radiation. So, if the need arises to get an MRI, take melatonin. For radiation therapy take several hundred mg of melatonin (from 100 to 200 mg) about an hour before your MRI. On average, the combined results of these studies show that melatonin reduces the death rate by a whopping 44%. These are from human studies.
Mitochondrial aspects of oncology
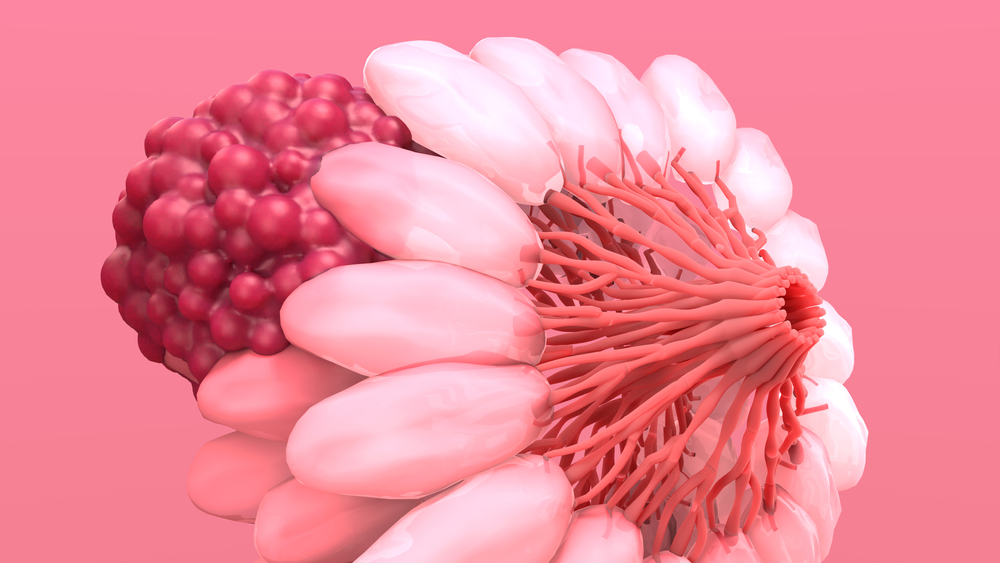
Because of its selective estrogen receptor modulators (SERM), selective estrogen enzyme modulators (SEEM), and its virtual absence of contraindications, melatonin could be an excellent adjuvant with the drugs currently used for breast cancer.
The antioxidant actions also make melatonin a suitable treatment to reduce oxidative stress associated with chemotherapy, especially with anthracyclines, and radiotherapy.
Melatonin’s anti-estrogenic properties are especially useful for breast cancer prevention in cases of obesity, steroid hormone treatment, or chrono-disruption by exposure to light at night even as little as a tiny fraction of (non-red) light.
The possible anti-cancer properties of melatonin on different types of neoplasias (abnormal growth) have been studied especially in hormone-dependent adenocarcinomas. Despite the promising results of these experimental investigations, the use of melatonin in breast cancer treatment in humans is still uncommon.
This article reviews the usefulness of this indoleamine (a family of neurotransmitters) for specific aspects of breast cancer management, particularly in reference to melatonin’s anti-estrogenic and antioxidant properties:
- Treatments oriented to breast cancer prevention, especially when the risk factors are obesity, steroid hormone treatment or chrono-disruption by exposure to light at night (LAN);
- Treatment of the side effects associated with chemo- or radiotherapy.
The clinical utility of melatonin depends on the appropriate identification of its actions. Because of its SERM and SEEM properties, and its virtual absence of contraindications, melatonin could be an excellent adjuvant with the drugs currently used for breast cancer prevention (antiestrogens and anti-aromatases). The antioxidant actions also make melatonin a suitable treatment to reduce oxidative stress associated with chemotherapy, especially with anthracyclines, and radiotherapy.
In another study, ER+ breast cancer rat model was established and then rats were randomly divided into five different groups as follows:
1) Control group,
2) Diss group,
3) Adriamycin (ADM) group,
4) Melatonin group, and
5) Melatonin combined with Adriamycin (M + A) group.
Tumor weights were significantly lighter in M + A group than those in ADM group. Under optical and electro-microscopy, tumor cell apoptosis was obviously increased in the melatonin group, and tumor cell injury was more severe in the M + A group than in the ADM group.
Decreased E-cadherin expression in cancer cells increases proliferation, invasion, and/or metastasis. Expression of E-cadherin was higher in melatonin group and M + A group than in other groups. The Melatonin group had the highest one-month survival rate (100%), there was the poorest life quality in ADM group, but the best life quality was in the melatonin group.
Melatonin enhanced the sensitivity of tumors to ADM and improve patient’s life quality
Acute tubular necrosis is a major side effect of cisplatin. Melatonin is a direct free radical scavenger and indirect antioxidant. We investigated the effects of melatonin on cisplatin-induced changes of renal malondialdehyde (MDA), a lipid peroxidation product, and blood urea nitrogen (BUN) and serum creatinine (Cr). The morphological changes in kidney were also examined using light microscopy.
Melatonin administration either before or after CDDP injection (see below) caused significant decreases in MDA. The morphological damage to the kidney induced by cisplatin was reversed by melatonin.
The results show that pharmacological and physiological concentrations of melatonin reduce cisplatin-induced renal injury. Melatonin is both a direct and indirect free radical scavenger. The radical scavenging ability of melatonin works via electron donation to detoxify hydroxyl radical. Ionizing radiation results in the production of hydroxyl radical.
The results from many in vitro and in vivo investigations have confirmed that melatonin protects mammalian cells from the toxic effects of ionizing radiation.
Furthermore, several clinical reports indicate that melatonin administration, either alone or in combination with traditional radiotherapy, results in a favorable efficacy: toxicity ratio during the treatment of human cancers.
Radiation-induced dermatitis is commonly seen during radiotherapy for breast cancer. In a randomized, placebo-controlled double-blind study, patients were allocated to a melatonin-containing topical cream twice daily during radiation treatment and 2 weeks following the end of radiotherapy.
Grade 1-2 acute radiation dermatitis was 59% vs. 90% in the melatonin group. Patients treated with melatonin-containing emulsion experienced significantly reduced radiation dermatitis compared to patients receiving placebo.
Dosing with Melatonin
- For prevention, take 180 mg about 45 minutes before bedtime every evening.
- If you have cancer, take 60 mg 3-6x/day (always work with a clinician).
- If you have a PET (Positron Emission Tomography) scan, take 300 mg two hours before.
Remember, there are no known contraindications for melatonin.
References
1.) Cowan T. Why melatonin helps resolve many disease processes. Fourfold Healing. June 20, 2019.
2.) Su SC, Hsieh MJ, Yang WE. Cancer metastasis: Mechanisms of inhibition by melatonin. Pineal Res. 2017 Jan;62(1).
3.) Mills E, Wu P, Seely D , Guyatt G. Melatonin in the treatment of cancer: a systematic review of randomized controlled trials and meta-analysis. J Pineal Res. 2005 Nov;39(4):360-6.
4.) Mediavilla MD, Sanchez-Barcelo EJ, Tan DX, Manchester L, Reiter RJ. Basic mechanisms involved in the anti-cancer effects of melatonin. Curr Med Chem. 2010;17(36):4462-81.
5.) Ma Z, Yang Y, Fan C. Melatonin as a potential anti-carcinogen for non-small-cell lung cancer. Oncotarget. 2016 Jul 19;7(29):46768-84.
6.) León J, Casado J, Jiménez Ruiz SM, Zurita MS, González-Puga C, Rejón JD, Gila A, Muñoz de Rueda P, Pavón EJ, Reiter RJ, Ruiz-Extremera A, Salmerón J. Melatonin reduces endothelin-1 expression and secretion in colon cancer cells through the inactivation of FoxO-1 and NF-κβ. J Pineal Res. 2014 May;56(4):415-26. doi: 10.1111/jpi.12131. Epub 2014 Apr 15.
7.) Reiter RJ. Mechanisms of cancer inhibition by melatonin. J Pineal Res. 2004 Oct;37(3):213-4.
8.) Sanchez-Barcelo EJ, Mediavilla MD, Alonso-Gonzalez C, Reiter RJ. Melatonin uses in oncology: breast cancer prevention and reduction of the side effects of chemotherapy and radiation. Expert Opin Investig Drugs. 2012 Jun;21(6):819-31.
9.) Ma C, Li LX, Zhang Y, Xiang C, Ma T, Ma ZQ, Zhang ZP. Protective and sensitive effects of melatonin combined with adriamycin on ER+ (estrogen receptor) breast cancer. Eur J Gynaecol Oncol. 2015;36(2):197-202
10.) Parlakpinar H, Sahna E, Ozer MK, Ozugurlu F, Vardi N, Acet A. Physiological and pharmacological concentrations of melatonin protect against cisplatin-induced acute renal injury. J. Pineal Res. 2002 Oct;33(3):161-6.